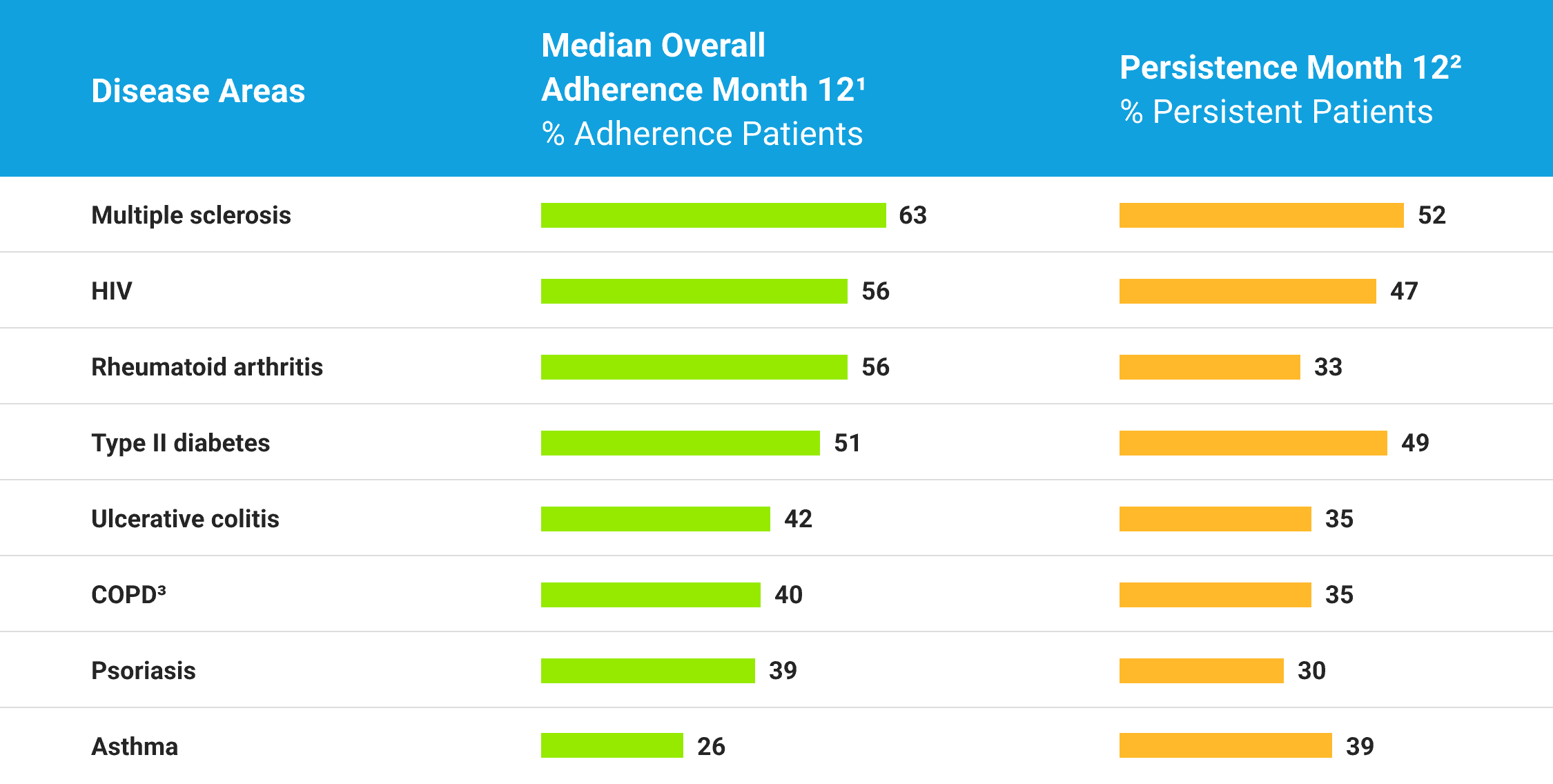
Living with a serious disease can be overwhelming. Despite best efforts, patients struggle to take their medication as intended: doses get missed, refills get delayed, or treatment stops entirely. Unfortunately, it takes about ten weeks to establish a new habit and only one week to lose it. 1,2
Traditional approaches to helping patients start and stay on their medication don’t work because they add to the burden or act too late. Oftentimes, these approaches are driven by dated prescription refill data and arrive when the medication-taking behavior has been broken. Newer methods, such as digital apps, suffer from low uptake and have no insight into the patient’s life arriving too late or too often, resulting in alert fatigue and patient disengagement.
1. Can the theory of planned behavior predict the maintenance of physical activity?
2. How are habits formed: Modelling habit formation in the real world